
Sophie's Story
Sophie weighed just 1 pound, 9 ounces when she was
born in August 2021, nearly four months premature.
Her whole body fit into her father’s palm. Her tiny
hand curled around the tip of his finger.
The fragile
newborn spent her first eight weeks in an incubator
in the Neonatal Intensive Care Unit (NICU) at the
IWK Health Centre in Halifax, connected to breathing
tubes and monitors.
Even after she could leave the incubator, Sophie had
to stay in the NICU as she fought to gain every ounce
of weight, connected to oxygen for 99 days.
For each
one of the 115 days she spent in hospital, her parents
fought alongside her, in their own survival mode.
“You are in that unit because your child’s life is in
danger,” says her mother, Emily. “Every day we spent
in that unit, we thanked science, we thanked whatever
it is that you believe in, for her life.”
Because Sophie was born at just 25 weeks gestation,
her healthcare team warned Emily and her husband,
Mark, that their baby would face intense oxygen
requirements. Sophie was at risk for a brain bleed,
heart problems, respiratory distress, lung disease or
intestinal issues.
It was not a question of whether she would encounter
one of those problems—the question was which one,
and how severely it would affect her. Her biggest
challenge was heart surgery.
Unlike in most full-term babies, an extra blood
vessel connecting two major arteries to carry blood
away from Sophie’s heart did not close on its own.
There was too much blood flowing into her heart,
straining her under-developed lungs and increasing
her blood pressure.
Doctors decided they had to intervene to close the
open vessel, or duct, called Patent Ductus Arteriosus.
Sophie weighed just two pounds when Emily and Mark
watched a team wheel her off to an operating room.
“It was the worst day of my life,” says Emily.
Every day, and during every new test, Emily willed
Sophie to hang on. She sang and whispered to her
baby: “You are strong, you are brave, you are kind, and
you are very cute.”
Finally, Sophie turned a corner following the surgery.
She began to add weight. Mark and Emily and their
mothers donned party hats. They celebrated every
ounce and every week Sophie gained.
Today, Sophie is a strong, happy two-year-old. A
healthcare team still follows her closely, but she is
meeting her developmental milestones and making
her parents proud and happy every day.
Sophie remains at risk for learning disabilities and
breathing issues, but Emily and Mark are thankful
for medical research and for the excellent care she
received from her hospital team that brought her
through those heart-stopping early months.
Now they hope the research Dr. Tobias Kollmann, Dr. Nelly Amenyogbe, and their colleagues are conducting will prevent other families from experiencing preterm births, and spare babies like Sophie from the struggle she experienced.


Born Strong
Did you know that stillbirths, premature births, and infections in infants are the main cause of death and disability for children?About eight percent of all live births in Canada are premature, which translates to about 28,000 babies born prematurely in the last year or so. Another 15-25 percent of all pregnancies end in miscarriages — a number that could be as high as 60,000 to 120,000 miscarriages per year in Canada. While there are approximately 3,100 stillbirths in a year, about 30 women die in childbirth or complications due to childbirth.
At Dalhousie University, Dr. Tobias Kollmann, a pediatric infectious disease specialist, is spearheading an initiative to improve the well-being of expectant mothers and their babies.
Together with a dedicated team of researchers, Kollmann is developing a revolutionary at-home monitoring system, like a smart watch, designed to evaluate a woman’s risk of delivering early or having other negative outcomes during pregnancy.
These portable devices, intended to be worn comfortably, will assess how the body utilizes nutrients and energy. By measuring the balance of carbon dioxide exhaled and oxygen inhaled, the system aims to detect subtle changes that may indicate potential risks or complications throughout pregnancy.
Dr. Kollmann and his team believe by tracking these changes remotely, they can empower local healthcare providers to intervene proactively, safeguarding the health of both mother and child. This innovative approach is particularly important for underserved communities, including Indigenous people residing in rural or remote areas, where access to comprehensive prenatal care may be limited.
Unlike traditional methods, which rely on costly and invasive blood tests done in clinical settings, this wearable system promises a more accessible alternative. Dr. Kollmann and his team envision a future where pregnancy care is personalized, non-invasive, and readily available to all, regardless of geographical location or socioeconomic status.
Dr. Kollmann and the team at Dalhousie need your help to conduct a pilot study involving pregnant women in Nova Scotia. This initial phase will provide invaluable data, paving the way for larger clinical trials and further exploration of innovative pregnancy monitoring technologies.
Give today and help us raise $75,000 towards transforming prenatal care, ensuring a brighter, healthier future for generations to come.
Meet the Researchers
Dr. Tobias Kollmann
Dr. Tobias Kollmann is a doctor who specializes in pediatric infectious diseases. He is a professor of microbiology and immunology at Dalhousie University and a member of the Inflammation, Infection, Immunology, and Vaccinology (I3V) research team. He is also the founder of the Born Strong Initiative, a network of scientists and researchers who are striving to transform maternal and child health around the world.
Dr. Kollmann’s research focuses on reducing maternal and child deaths by strengthening the immune system of pregnant women and babies, developing remote home monitoring systems to help prevent preterm births, and empowering underrepresented communities. His goal is to increase diverse representation in all stages of research, from discovery to delivery.

Dr. Nelly Amenyogbe
Dr. Nelly Amenyogbe is a postdoctoral research fellow at Dalhousie University, working with the I3V group – Inflammation, Infection, Immunology, and Vaccinology. She investigates the molecular, genetic, and environmental factors that affect an infant’s resistance to infection. Her projects include deciphering the influence of colostrum and studying the beneficial effects of a tuberculosis vaccine called Bacillus Calmette-Guérin (BCG) on babies’ immune systems.
Amenyogbe, who is of West African heritage, received a Canadian Institutes of Health’s Research Excellence, Diversity and Independence (REDI) Early Career Transition Award in 2023. The REDI awards support clinicians, researchers, and postdoctoral students from underrepresented groups as they launch their research careers.

About Molly Appeal
The Molly Appeal is Dalhousie University's annual campaign created to raise critical funds throughout the year in support of local health research excellence.
Molly Moore was a real person who held the spirit of philanthropy in her heart; she also cared deeply about local health research. Over 40 years ago, Molly took a simple but dramatic step. She gave five dollars to Dalhousie Medical Research Foundation (DMRF). While not a woman of great means, she believed that if everyone made a gift to support medical research, together we could make a big difference. Molly's remarkable first step inspired DMRF to launch the annual Molly Appeal campaign in her honour. Molly continued to give what she could throughout her life.
"Research is the best medicine." - Molly Moore
Your gifts to the annual Molly Appeal support health research right here in the Maritimes. Molly's commitment continues to inspire thousands of people to give to the annual appeal, which has raised over $6 million to date.

Previous campaigns
-
2022: Spring Molly: Youth Mental Health

This spring, Molly is raising funds in support of mental health research for youth. We all know how important mental wellness is at any age, but especially during our developmental years. And let's face it, young people have experienced extraordinary times as living through a global pandemic has seen them home-schooling, isolating away from friends, missing out on extra-curricular activities, masking-up, and worrying about health issues that usually never would have come to mind.
Dalhousie researcher and child and adolescent mental health researcher, Dr. Leslie Anne Campbell, understands all too well the critical importance of mental health for young people. While the pandemic opened many virtual doors when it came to accessing mental health services, digital options were found to not always be the best choice for everyone. Dr. Campbell wants to find solutions that provide the easiest access and the best care to young people struggling with their mental health.
And that's what the spring Molly is all about.
Dr. Campbell and her team are working hard to develop a tool that will enable them to best determine whether virtual care or in-person care is the optimum option for a young patient. This dynamic and caring group of researchers are creating a science-based decision-making tool that will help young people, parents, and care providers choose the best care model that will lead to the best mental health outcomes!
We think that's exciting.
When Molly Moore donated five dollars to medical research more than 40 years ago--and launched the treasured Maritime tradition of the Molly Appeal--I don't think she could have imagined the virtual care options we have now. But Molly believed that "research is the best medicine," and that is still the case today".
- Dr. Leslie Anne CampbellMeet our researcher
Child and Adolescent Mental Health Researcher, Dr. Leslie Anne Campbell
Dalhousie Medical School's researchers are passionate in their pursuit of answers. They are making critical discoveries that are bringing us closer than ever to lasting cures for a wide range of devastating diseases and conditions. In doing so, they are truly taking Molly’s mission into the 21st century. Molly Appeal Researchers include Dalhousie Medical School’s researchers and students, striving for cures with support from Dalhousie Medical Research Foundation donors.
MORE ABOUT DR. CAMPBELL
Dr. Leslie Anne Campbell is the Sobey Chair in Child Adolescent Mental Health Services, and the lead researcher for Mental Health Services Research for Children & Youth Mental Health. Dr. Campbell is in pursuit of health care solutions that provide the easiest access and the best care to young people struggling with their mental health.
As a member of the Faculty of Health and Medicine at Dalhousie University and having begun her health care career as a public health nurse, Dr. Campbell has found herself face to face with the complications of managing mental health amidst our younger population. So, she decided to address it.
Dr. Campbell’s research focuses on examining the functions of the current health care system to ensure that the right systems are in place, and to evaluate if those systems are functioning at their full capacity. Her research asks questions such as: Are we offering the optimal services for addressing youth mental health? The COVID 19 pandemic has led to many shifts in the way health care services are offered, including the ways in which we are providing virtual care.
“We can only treat those that we can get in the door, and sometimes that door is exclusively virtual”
In an effort to prove that there have been outweighing benefits to this shift, it’s important to understand what possible barriers will exist when it comes to establishing a virtual care framework for youth mental health. Virtual care allows for better access to care, ideally, however there are inevitable barriers including but not limited to access to private space, bandwidth, or access to technology. Dr. Campbell believes that starting to focus on youth means a healthy future for all, and that with the right support and research, we can establish a health care system that provides client-centered treatment options, specifically for youth mental health.
Youth should be able to access the care they need, when they need it, where they need it.
With funding, Dr. Campbell’s research will provide the opportunity to develop a ‘tool’, to gauge the needs and requirements for establishing a successful youth mental health virtual care system tailored for successful outcomes. At this point, we understand that virtual care works for some, but we know it does not work for all. It must be an option, but only with further research will we understand what and how to offer care options that are ‘best’ for the youth in our province.
"We all know mental health is complex, and the answers to these questions aren't easy. The problem is, right now, there are no guidelines to help families and doctors determine when or if to use virtual care--and when in-person care might be the better choice."
WHY WE NEED YOUR SUPPORT
Keegan's Story
I am a mom to seven-year-old twins. Like many, our family experienced a lot of challenges throughout the pandemic. My son Keegan, especially, really struggled with online learning. Over time, I noticed that he was becoming fixated and worried about things that a little boy shouldn’t even be thinking about—like death and dying. His teachers were also pointing to a number of learning challenges that were amplified during remote learning.
Our family doctor and I decided to have Keegan assessed, and it turns out that he has generalized anxiety disorder and ADHD—a very heavy burden for such a sweet little boy. I am so grateful that we have a treatment plan in place, and that there are medications that can help ease his mind. Now he can just enjoy being a kid. None of this would be possible without medical research.
Mental illness runs in my family. It means so much to me to be able to access this type of early intervention for my son.
DMRF is the bridge between the community and the researchers who work to crack the code on mental illness for people like Keegan. I’m so grateful that this work is being done to strengthen youth mental health support in our community. Your support of DMRF truly means the world to me and my family—thank you.
-
2021: Fall Molly: Biomaterials Innovations Research
BIOMATERIALS INNOVATIONS RESEARCH
Last fall, DMRF Molly donors came together to support life-saving biomaterials research. This type of research is changing the face of how we treat a vast array of diseases and conditions. DMRF is inspired by how biomaterials can minimally target and treat dental decay, osteoarthritis, wounds, and certain cancers. Special thanks to the researchers at Dalhousie University’s Faculty of Dentistry, who are dedicating their time to advancing this critical area of research. They believe that biomaterials will offer patients precision treatment options that are not only less invasive, but progressively impactful.
Special thanks to featured researchers:
- Dr. Daniel Boyd
Associate Professor, Department of Applied Oral Sciences, School of Biomedical Engineering - Dr. Mark Filiaggi
Professor, Faculty of Dentistry, School of Biomedical Engineering - Dr. Tsanka Todorova
DMRF Research Fellow in Osteoarthritis - Brenna Kettlewell
DMRF Conrad Studentship recipient - Robert (Bob) Abraham
Professor, Department of Diagnostic Radiology
“I want to send a special thank you to all the DMRF Molly Appeal donors. Your generosity will help support the creation of a biomaterials innovation lab that will be a game-changer for our region when it comes to ground-breaking health research outcomes. We all deserve good health and I promise to work hard to make this a greater reality for each of us”.
- Dr. Daniel Boyd
Associate Professor, Department of Applied Oral Sciences, School of Biomedical Engineering, Dalhousie University - Dr. Daniel Boyd
-
2020: COVID-19 Research
JOIN US IN THE GLOBAL FIGHT AGAINST COVID-19
Dalhousie University is a global leader in the discoveries and development of new vaccines, antiviral drugs and other life-saving viral therapies. And now, Dalhousie researchers are using their knowledge and expertise to focus on the fight against COVID-19.
Dalhousie researchers are collaborating with experts around the world to fight COVID-19, and have already mobilized on a number of projects that will be so essential in the weeks and months to come. The number one priority of course is to find COVID-19 vaccines that will bring this pandemic under control. And, they’re also working on other critical projects like new antiviral drugs, anti-inflammatory drugs to treat COVID-19 pneumonia and the development of rapid response test kits.
Dalhousie Medical Research Foundation is proud to support this essential research, with the help of our generous community of donors.
Canadians from coast to coast are counting on our research community to find the solution. Let’s show the world what we can do when we all pull together.
-
2019: Mass Spectrometer
Like Molly Moore, we know that every gift makes a difference and when it comes to health research, your gift has the ability to change and save lives. Our researchers work tirelessly to establish solid preventative measures, faster diagnosis, better and more personalized treatments and, ultimately, cures for the conditions and diseases that effect everyone. You, as a donor, are a part of our vision to create a world where good health, both mentally and physically, are a reality for all; health research is the key.
What we're fundraising for

You can never truly be prepared to hear that your son’s or daughter’s heart has stopped. Mother Wendy Coley knows this all too well. Last November, her son Curtis was in a serious car accident that stopped his heart, twice.Dr. Rob Green, a trauma and critical care provider knows that time is of the essence with treating someone like Curtis. With a severe brain injury like Curtis’, the traditional course of treatment is heavy sedation. But Dr. Green's experience taught him that a patient’s overall condition doesn’t improve very quickly under sedation.
The mass spectrometer that DMRF's Molly Appeal is fundraising for could have provided the science necessary to ensure Dr. Green and his team made an accurate and timely decision regarding Curtis' recovery; instead, they had to wait two months and then make that crucial choice.
Thankfully, Dr. Green and his team's experience led them to taking Curtis off of sedation and he made a slow but steady recovery.
This holiday season, Mom Wendy's greatest gift is sharing this special time of year with her son.
As donors, you can play a big part in helping our researchers develop more effective personalized treatment plans and improve the lives of people like Curtis.
We need your help to reach our $251,082 goal.
Curtis’ story is just one example of what advances in medical research can do. Your continued generosity will help save lives and improve the quality of life for people throughout the Maritimes and beyond.
- Dalhousie Medical Research Foundation’s fall 2019 Molly Appeal is set to equip Dalhousie’s Faculty of Medicine’s leading research teams with a sophisticated device that will open up a whole new scientific frontier in eastern Canada.
- The Orbitrap Fusion Mass Spectrometer will improve our ability to advance personalized cancer treatments, as each patient’s cancer is different. Not only that, this equipment can help research in MANY health conditions and diseases.
- The mass spectrometer will allow us to analyze cells and discover how they fight disease. This equipment is vital in our efforts to learn how to train our immune system to fight cancer.
- This powerful equipment will transform our ability to diagnose and treat cancer and other diseases.
- With support from donors like you, we will have the mass spectrometer working in our labs within the year!
Your gift today will help bring hope and better outcomes to the many people facing trauma, cancer and many other challenging diseases and conditions. And your donation towards this equipment will accelerate the pace of our research and lead us to breakthroughs sooner.
Here’s what your donation will do.
- The mass spectrometer is imperative to all health research. Not only will it be used in cancer research, but it is essential to so many researchers searching for treatments and cures for all diseases and conditions at Dalhousie’s Faculty of Medicine.
- The Orbitrap Fusion Mass Spectrometer will replace 20-year-old technology to provide researchers with the most powerful tool available for analyzing proteins and the by-products of metabolism in cells, rapidly and precisely.
- This will shed light on the mechanisms of a vast range of diseases, including cancer, Alzheimer’s disease, ALS, autoimmune diseases, infectious diseases, bipolar disorder, and schizophrenia.
- The Orbitrap Fusion Mass Spectrometer is up to 100 times more sensitive than the technology it will replace, giving scientists dramatically more detailed information about the workings of proteins and metabolites in the body, and paving the way to new strategies for diagnosing and treating disease.
The new equipment will position Dalhousie medical researchers to be international leaders in the emerging and influential field of proteometabolomics, which studies the impact of both proteins and metabolites on cell function in health and disease!
-
2019: Cardiovascular Research
More than 35 years ago Molly Moore took a simple but dramatic step. She gave five dollars to Dalhousie Medical Research Foundation (DMRF). While not a woman of great means, she believed that if everyone made a gift to support medical research, together we could make a big difference. Molly's remarkable first step inspired DMRF to launch the annual Molly Appeal campaign in her honour. Molly continued to give what she could throughout her life.
100% of every gift to the annual Molly Appeal supports medical research at Dalhousie Medical School right here in the Maritimes. Molly's commitment continues to inspire thousands of people to give to the annual appeal, which has raised over $5 million to date.
Molly's Appeal for Mother's Day

This Mother's Day the Breen-Porter family is celebrating together thanks to the great strides made by medical research supported by people like you. Mother Kaitlin shares the touching story of her youngest daughter Everly, who was born with a congenital heart disease that could have taken her life; for a while, they didn't know if she would survive.This Spring, we are raising funds to support critical heart research, right here at Dalhousie's Faculties of Medicine in Nova Scotia and New Brunswick. Our researchers want to reduce heart disease locally and around the world. You can help us reach our $100,000 goal, that will help us expand biobank facilities. This biobank will ehance our capacity for sample and data collection, which strengthens collaborative research. The biobank houses heart tissues and health information from patients, providing a rich resource for cardiovascular researchers at Dalhousie Medical School in New Brunswick and Nova Scotia.
Together, we CAN make a difference.
You, as donors, are a critical part of the team that keeps babies like Everly strong and healthy and able to enjoy a beautiful Mother's Day with her family. Thank you for your support!
The Maritimes are home to the highest rates of heart disease in Canada, as well as the highest rates of such important risk factors as older age, frailty, obesity and diabetes. Dalhousie’s growing team of heart researchers is investigating how these factors contribute to heart disease—including a poorly understood form of heart failure known as diastolic heart failure that affects more women than men.
Dalhousie’s cardiovascular researchers will use the biobank to learn what drives the development of diastolic heart failure—and other forms of heart disease—and to explore potential new cures. Our researchers are investigating many different angles—such as the effect of sex hormones, exercise, age, frailty and metabolic disorders on the development of heart disease. They are even studying how the heart adapts to the demands of pregnancy, to see if any of these mechanisms could be harnessed as a treatment for heart failure. Together, their heartfelt desire is to save and improve the lives of the thousands of Maritimers.
-
2018: Molly's Holiday Campaign
A Special Holiday for Baby Ella and Her Family

During the Holiday Season, our family celebrates Christmas. Spending last Christmas in the hospital was heartbreaking for our family. You see, our youngest daughter Ella had been diagnosed with childhood leukemia just a couple weeks earlier. Ella wasn’t able to leave the hospital. This was very hard to explain to her big sister, Marin. She was very worried that Santa wouldn’t be able to find them.We tried to keep some of our traditions alive – decorating a tree in Ella’s hospital room, and leaving out milk and cookies for Santa and the reindeer.
But there were a lot of traditions that we missed. Going as a family to pick out our Christmas tree. Counting down the days until Santa came. Marin especially loves baking gingerbread people and would have written her first letter to Santa. But none of that was possible.
It obviously wasn’t the Christmas we hoped for. Both my husband and I are from big close-knit families in PEI. It was the first time in years that we hadn’t been able to travel for our family Christmas gatherings. But I think our girls still had fun, despite missing family.
I’m glad to tell you that since then things have improved a lot for our daughter Ella, thanks to research made possible through the Dalhousie Medical Research Foundation (DMRF). I’ll tell you more about her journey with leukemia in a moment, but first I want to let you know why I’m sharing this story with you today.
I volunteered to write this letter to you on behalf of the DMRF. You’re probably familiar with their Molly Appeal. Contributions from generous people like you fund life-saving research that helps people right here in the Maritimes. This includes our daughter Ella. And once I’ve told you more about the research they did to help our little girl, I hope you’ll make a donation to support this work today.
When we first met Dr. Jason Berman we were so impressed. He was chairing an international study on kids with childhood leukemia. We agreed to take part in the study – the first ever clinical trial providing tailored treatments to each child. We felt so lucky and so blessed to have Ella as part of the study.

Ella responded well to her first round of chemo. Her more personalized approach worked. Her energy and appetite were pretty good, and she only lost her hair after the last round of chemo.Ella’s condition has continued to improve and her cancer is in remission today. She still needs to be in the hospital for a few weeks of chemo this year, as a preventative measure. But thankfully, because of the amazing research funded by DMRF donors like you, she has a chance of a complete and permanent cure.
So, with Christmas so close, we hope she’ll be able to spend Christmas at home this year. It’s such a magical time, especially for children who love decorating, baking, and putting up stockings. And of course the presents and parties.
To be able to have Christmas at home with both of our daughters, and family, is the greatest gift of all.
You might not realize it, but you’ve played a big part in making this happen. Donors like you are critically important to the research conducted by Dr. Berman, and the many other amazing doctors and researchers.
We’re truly honoured to be part of this year’s Molly Appeal. The Dalhousie Medical Research Foundation has really been there for us and our daughter. The research, that you helped to fund, has helped our little girl.
So I want to say thank you! You are changing lives. You are having a positive effect on families like ours. And today, I hope you will make a donation to the DMRF to help another family. Any amount you choose to give can make a life-saving difference.

Whatever you celebrate this season, we wish you happiness and joy,
Rebecca Martin-Fraser
Ella’s grateful motherP.S. You may be aware that the Molly Appeal is named after Molly Moore. She believed that scientific research would lead to life-saving cures. And she was so right! Thanks to donors like you, there have been many amazing breakthroughs.
P.P.S. This year we’ll start a new family tradition. We will visit other kids in the hospital over Christmas to give them gifts, and brighten their spirits. I hope you’ll join us in this season of giving by making the most generous donation you can to DMRF today. Your gift will help produce the next breakthrough and help more families like ours.
-
2018: I3V and Genomics
2018 Molly Appeal for I3V and Genomics
What we're fundraising for

Dalhousie Medical Research Foundation’s 2018-19 Molly Appeal will provide matching funds to allow Dalhousie Medical School to acquire a very important new piece of equipment that will be used by researchers in dozens of labs at Dalhousie Medical School. The equipment is the ImageStreamX Mark II, a state-of-the-art hybrid instrument that combines microscopic visualization of individual cells with the ability to analyze five thousand cells per second by flow cytometry (high-speed cell sorting).Conventional cell-analysis equipment only allows researchers to look at cells as groups, to see what is happening in populations of cells “on average.” The ImageStreamX Mark II will allow the researchers to isolate individual cells that exhibit unusual behaviours. These rare cells may be the keys that unlock the secrets of many diseases and lead the way to new cures.
The ImageStreamX Mark II will be a powerful discovery tool. It will allow Dalhousie medical researchers not only to better understand cellular and microbial processes in health and disease, but also to identify targets for new therapies and monitor the effects of experimental and existing drugs on a wide range of diseases.
-
2017: Cancer Research
The 2017 Molly Appeal was dedicated to collaborative cancer research at Dalhousie Medical School and its affiliated teaching hospitals.
We are pleased to be working with Dr. Paola Marignani and a team of over 15 astounding medical researchers, for this year's Molly campaign.
Click on the video below to learn more about this cutting-edge project:Dr. Paola Marignani, Professor, Department of Biochemistry & Molecular Biology and Department of Pathology Dalhousie University Medical School
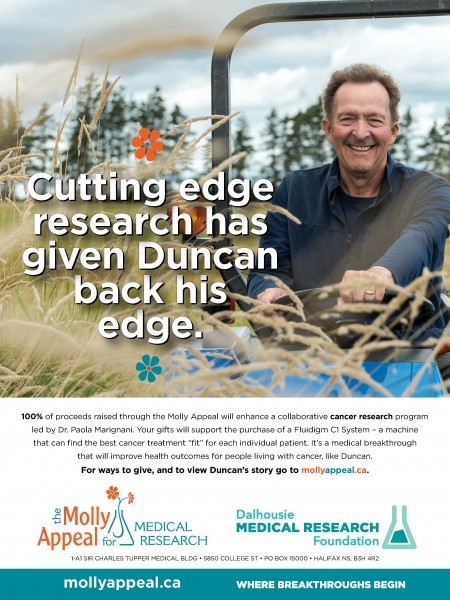
Advances in research will lead to better diagnoses and treatments for patients with many types of cancer. Please give generously to this year's Molly Appeal and help researchers who are working to understand the complexities of cancer and provide personalized precision care and improved quality of life for patients and their families.Faces of Molly 2017-18
Dr. Drew Bethune helps launch molecular testing for precision treatment of cancers
Dr. Jeanette Boudreau programs NK cells to kill virus-infected and cancerous cells
Dr. Carman Giacomantonio & Dr. Paola Marcato take aim at the bad guys
Dr. Wenda Greer reveals cancer' unique features to guide personalized treatment
Dr. Paola Marignani seeks personalized treatments for high-mortality cancers
Dr. Zhaolin Xu establishes Canada's largest, most comprehensive lung cancer tissue bank -
2016: Inflammation, Infection & Immunity Research
2016-17 Molly Appeal for Inflammation, Infection and Immunity Research
This year's Molly appeal is dedicated to collaborative research in the vast area of inflammation, infection and immunity.
At some point in our lives we all face issues in these areas, regardless of age, ethnicity, gender or geography.Dr. Andrew Makrigiannis Letter 2016-17 Molly Appeal for Inflammation, Infection and Immunity Research (PDF)
Theresa Morley Letter 2016-17 Molly Appeal for Inflammation, Infection and Immunity Research (PDF)
Advances in research will lead to better understanding, diagnosis, treatment and prevention for many complex and related conditions.
Please give generously to this year's Molly Appeal and help researchers unlock the mysteries of inflammation, infection and immunity and improve quality of life for all of us and our families.Faces of Molly 2016-17
Dr. Anil Adisesh explores health effects of workplace exposures
Dr. Lisa Barrett explores new approaches to rejuvenating worn-out immunity
Dr. Jeanette Boudreau programs NK cells to kill virus-infected and cancerous cells
Dr. Beata Derfalvi explores treatments for pediatric immune diseases
Dr. Thomas Issekutz gets to bottom of immune deficiency and autoimmune disorders
Dr. Morgan Langille leads initiative for computer analysis of the microbiome
Dr. Andrew Makrigiannis helps Natural Killer cells destroy harmful targets
Dr. Jean Marshall explores ways to prevent allergies, cancers and inflammation
Dr. Andrew Stadnyk turns pro-inflammatory cells into anti-inflammatory agents
Dr. Johan Van Limbergen searches gut bacteria for clues and cures to Crohn’s diseaseDid You Know?
Each year the Molly Appeal focus alternates on a rotating basis for the four key areas of research emphasis and excellence at Dalhousie Medical School: the related areas of Inflammation, Infection & Immunity, Cancer, Neuroscience and Cardiovascular.
Learn about the many research initiatives happening in the Maritimes at Dalhousie Faculty of Medicine in Nova Scotia and in New Brunswick at Dalhousie Medicine NB (DMNB) by reading our Faces of Molly section.

